Benefits for people, by people
At Chard Snyder, we do more than administer benefits and compliance services. We provide partnership with a higher purpose—simplifying life for employers, and helping participants make the most of their benefits and save for healthcare needs.
Our expert team is supported by advanced technology that ensures ease and efficiency. The result is a simple, smooth experience employers and plan participants can count on. That's our promise as we aspire to make a difference for others, every day.
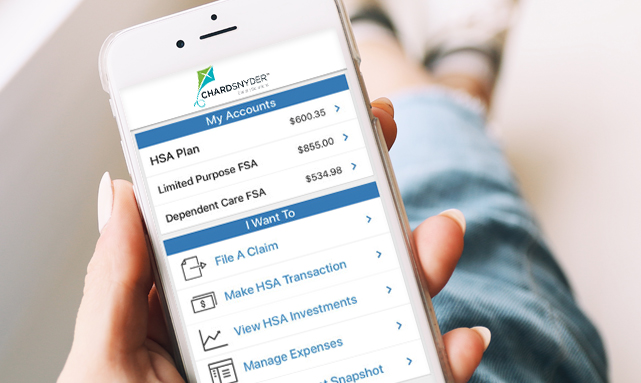
Mobile App
The Chard Snyder Mobile App provides a simple, easy way to manage your Chard Snyder savings and spending accounts from anywhere. Designed for convenient on-the-go access, our mobile app lets you securely view account balances, submit claims, send payments, manage expenses, and even scan items for eligibility with the touch of a finger.- Employees
- Employers & Advisors
We know navigating the world of employee benefit plans can be overwhelming and you likely have questions. We’ve simplified the process and our tools to help make it easier for you. You can find answers in our Support Center or if you’d rather talk to a person, give us a call.
We provide expert benefits administration services for clients nationwide, from small businesses to large employers across a wide variety of industries. We offer one-stop shopping for the most popular employee benefits to save you time, meet your unique needs, and make things easy and convenient for plan participants.
Everyone on the Chard Snyder team is responsive, kind, and very helpful to our staff and former employees/retirees. They are great at helping me understand things, provide great customer service, and are easy to work with. Our support person for COBRA and retiree billing is outstanding.







